Prior Authorizations
Before providing treatment or prescribing medication for an HPSM member, you may need to get prior authorization from HPSM to ensure that the treatment or medication is covered. HPSM expects providers to obtain authorization for services requiring prior authorization before they provide the service (with the exception of urgent and emergency services).
HPSM decides which services need prior authorization based on medical necessity. That is, the requested service must be safe, effective, reasonable and necessary to protect a person’s life, keep them from becoming seriously ill or disabled, or alleviate severe pain
HPSM generally does not require prior authorization for secondary claims that have been successfully processed and paid for by a member’s primary carrier, even for codes that are on HPSM’s prior authorization required list – learn more.
Use the search tool
This search tool includes all current CPT codes that require prior authorization. If the code you look up appears in the search results, you must complete and submit a Prior Authorizations Request Form. Wait for authorization approval from HPSM before providing the service to the member. Codes are updated quarterly
Log in to our provider portal to check the status of an authorization request. Provider Portal
PDF PAR Code Lists
Only CPT codes that require prior authorization are listed in these PDFs. Codes that are not on these lists do not require prior authorization. To use these lists offline, download and save the PDFs to your computer or device.
Medical PAR list
Prior Authorization Request Forms
Medical authorizations
Please make sure you complete our prior authorization form and that it meets the following requirements – failure to do so will result in a rejected request:
- Use the current Prior Authorization Request Form (version 5.0 January 2023)
- Use the fillable form (typed, not hand-written).
- Do not select “Urgent” unless it’s truly an urgent matter. Most requests will be “Routine” requests.
- Do not check the “LTC” box unless you are truly a long-term care provider or facility.
- Please make sure Prior Authorization form is the first page when faxing your request. Clinicals should be attached after the Prior Authorization form. Also: no coversheet is needed.
Physician Administered Drug (PAD) authorizations
Physician administrated drugs may require prior authorization request. For more information, please refer to the Medical Authorization lists.
Dental authorizations
Primary care dental providers and specialty dental providers who identify a need for dental services that require prior authorization for an eligible HPSM member should complete an American Dental Association 2019 dental claim form (any ADA form version after 2012 will also be accepted, as well as Medi-Cal Dental TAR form). The prior authorization is used to determine a member’s eligibility for services requested.
Additional information is requested to make determination which can include but not limited to: dental x-rays, dental images, periodontal chart, and/or a narrative.
All dental prior authorizations can be sent electronically or by mail.
Mailed authorizations
HPSM Dental
PO Box 1798
San Leandro, California 94577
Electronic authorizations
Clearinghouse information:
Payer Name: Health Plan of San Mateo Dental
Payer ID: HPSMD
Response times
For authorization requests submitted prior to the date of service, expect a response from HPSM:
- 72 hours for urgent (a delay in care could seriously jeopardize the life or health of the patient or the patient's ability to regain maximum function and/or a delay in care would subject the member to severe pain that cannot be adequately managed without the care or treatment requested in the prior authorization).
- 5 business days for routine (all other requests).
Your PAR will be rejected if you submit:
- An outdated version of the form.
- An incomplete form.
- Inaccurate information.
- A form filled out in handwriting.
- A PAR with multiple patients’ information.
Before submitting a request form, search HPSM's prior authorization list by code or service name to see if prior authorization is required. Learn more about the temporary changes to authorization requirements due to COVID-19.
HPSM regularly updates our list of authorization codes to reflect current clinical guidelines. Archived lists are published on our PAR List Changes page.
Inpatient Authorizations
- For all inpatient admissions, HPSM should be notified within 24 hours or the next business day.
- For admission notification, fax face sheet to 650-829-2060. When attaching clinical information, please place the face sheet before the clinicals.
- Do not submit notification for admissions to observation status. Observation status is direct billable.
- Do not submit requests for services delivered in the emergency room. Emergency room services are direct billable.
- Clinical information for concurrent review should be faxed to 650-829-2068
Authorization Fax Numbers
HPSM has several direct fax lines dedicated to specific form submissions:
|
In-patient admissions with facesheet for all lines of business (including in-patient retros and corrections): |
650-829-2060 |
|
In-patient admissions, clinicals only (without facesheet) |
650-829-2068 |
|
Out-patient retro authorizations and corrections |
650-829-2079 |
|
PCP referrals for Behavioral Health and Recovery Services |
650-596-8065 |
|
Pharmacy authorizations and modifications to formulary |
650-829-2045 |
|
CBAS and MSSP referrals, Care Coordination |
650-829-2047 |
When including clinicals:
- Place the facesheet before any clinical information
- Do not submit observation requests: observation status is direct billable
- Do not submit requests for services delivered in the emergency room: these are direct billable
Standard Prior Authorization Requests
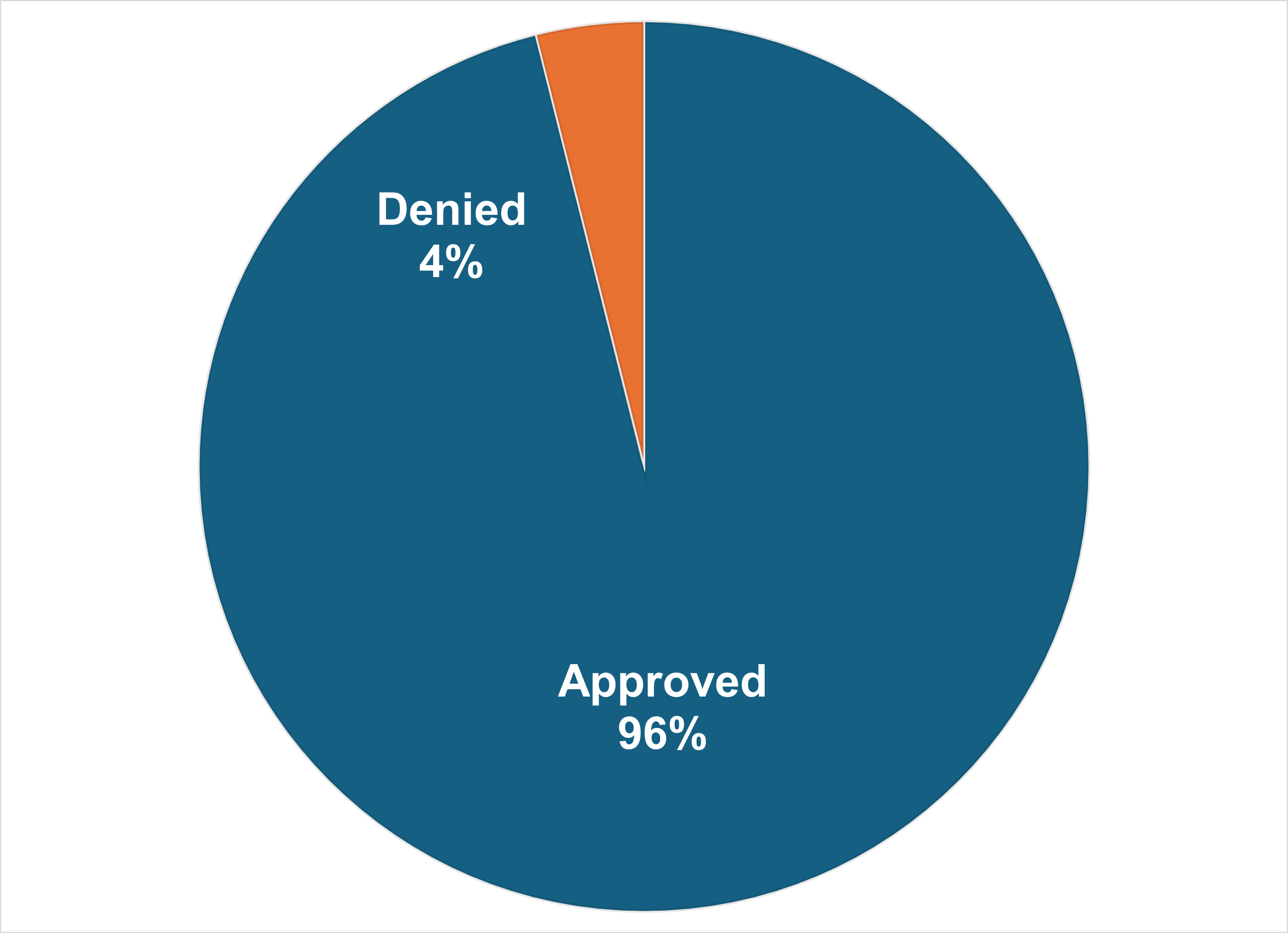
Responses to standard (non-urgent) prior authorization are due to providers within seven (7) calendar days. In 2025 we received a total of 8677 standard prior authorization requests for our covered patients. 96.1% of those requests were approved.
- Mean (average) time to make decisions: 2.8 days
- Median (middle) time to make decision: 2 days
Expedited Prior Authorization Requests
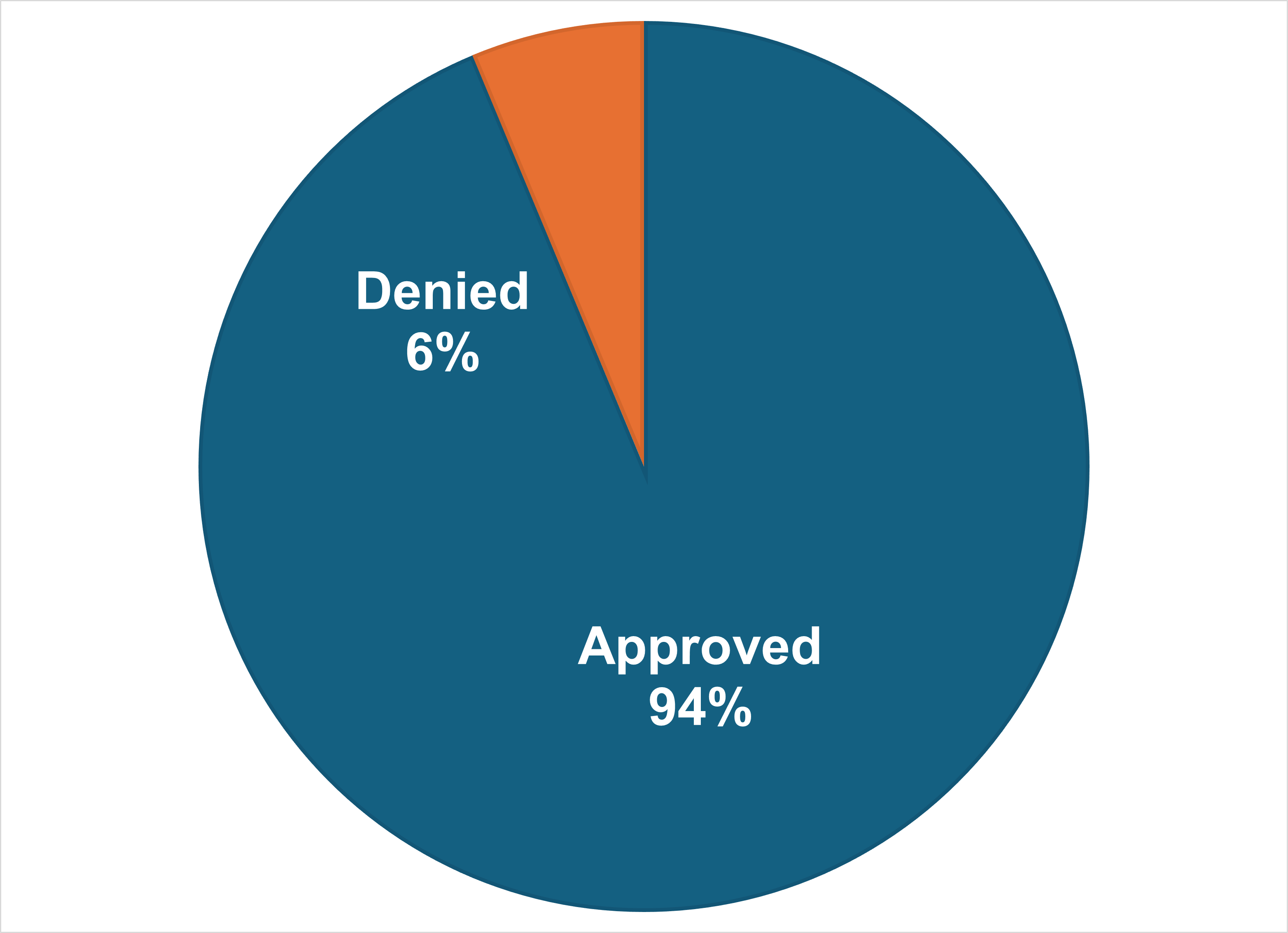
Responses to expedited (urgent) prior authorization are due to providers within three (3) days. In 2025 we received a total of 589 expedited prior authorization requests for our covered patients. 93.7% of those requests were approved.
- Mean (average) time to make decisions: 1.3 days
- Median (middle) time to make decision: 1 day
Frequently Asked Questions
The servicing provider should submit the prior authorization.
Retrospective authorization requests are reviewed to determine if the service was medically necessary using the clinical information submitted by the provider. Providers must also submit documentation about why the request was unable to be submitted prospectively.
Retrospective reviews for inpatient services with appropriate documentation will be accepted up to six months from the date of admission. Retrospective reviews for outpatient services must be submitted, with appropriate documentation, no later than 1 year from the beginning date of service.
Retrospective authorization decisions shall be communicated to the member who received the services, or the member’s designee, within 30 days of the receipt of information that is reasonably necessary to make the determination, and shall be communicated to the provider in a manner that is consistent with current regulations.
Please check our Prior Authorization Required list above.
Yes, the status of your authorization requests can be viewed in the Provider Portal.
Existing users login here.
New user? Register here or by calling 650-616-2106.
Please complete a Authorization Correction Form.
In the comment box on the prior authorization form, include a note indicating that a Letter of Agreement (LOA) is needed.
Please check your fax machine. If you have not received your letter within two days after our turnaround times, please contact the Prior Authorization Department at 650-616-2070 to have one faxed to you.
Facesheets should be faxed to 650-829-2060.
