Provider Manual | Section 2
Customer Support
Customer Support
The Health Plan of San Mateo (HPSM) provides customer support to its members through two dedicated call centers. The Customer Support staff can assist members who have questions about:
- HPSM coverage and benefits.
- Selecting or changing a primary care provider (PCP).
- Problems or complaints getting healthcare, pharmacy services, or billing issues.
The Member Services Department assists members that are enrolled in the Medi-Cal, HealthWorx and San Mateo County ACE programs.
- Members can call 1-800-750-4776 or 650-616-2133. Hearing impaired members can use the California Relay Service (CRS) at 1-800-735-2929 (TTY) or dial 7-1-1.
- Office hours are Monday through Friday, 8:00 AM to 4:00 PM.
- Phone hours are Monday through Friday, 8:00 AM to 6:00 PM.
- Member Services Customer Service Navigators speak Cantonese, English, Mandarin, Spanish, and Tagalog and can access telephone interpreters to assist members with other language needs.
The Medi-Cal Rx Customer Service Center can assist members enrolled in the Medi-Cal program regarding their pharmacy benefits (for all non-pharmacy-related questions, please refer to the Member Services Unit).
- Members can call 1-800-977-2273.
- Lines are open 24 hours a day, 7 days a week.
The CareAdvantage Unit assists members who are enrolled in CareAdvantage Dual Eligible Special Needs Plan (D-SNP). CareAdvantage is HPSM’s Medicare Advantage-Prescription (MA-PD) plan.
- Members can call the CareAdvantage Unit at 1-866-880-0606 or 650-616-2174, Monday through Sunday from 8:00 a.m. to 8:00 p.m. Hearing impaired members can use the California Relay Service (CRS) at 1-800-735-2929 (TTY) or dial 7-1-1.
- Office hours are Monday through Friday, 8:00 AM to 4:00 PM.
- CareAdvantage navigators speak Cantonese, English, Mandarin, Spanish, and Tagalog and can access telephone interpreters to assist members with other language needs.
HPSM members can also use the Member Portal to change their primary care physician (PCP), order a new ID card, change their address on file, and check their immunization records here.
HPSM mails each new member a New Member Guide that includes the ID Card for their assigned program and Materials Request Form to request member materials. The member materials that can be requested are summary of benefits, the member handbook, the provider directory, and formularies for CareAdvantage, HealthWorx, and ACE. For copies of materials related to Medi-Cal Rx, members can visit medi-calrx.dhcs.ca.gov.
Member Rights and Responsibilities
Member Rights and Responsibilities are established by the Centers for Medicare and Medicaid Services (CMS), DHCS, and HPSM Policies and Procedures.
HPSM members have these rights:
- To be treated with respect and recognition of your dignity, giving due consideration to your right to privacy and the need to maintain confidentiality of your medical information.
- To be provided with information about the plan, its services, practitioners, and providers, including covered services and member’s rights and responsibilities.
- To be able to choose a primary care provider within HPSM’s network (unless you have other primary health coverage).
- To participate in decision making with your providers about your own health care, including the right to refuse treatment.
- To voice complaints, either verbally or in writing, about the organization or the care received. • To receive care coordination.
- To request an appeal of decisions to deny, defer or limit services or benefits.
- To receive oral interpretation services for your language.
- To receive free legal help at your local legal aid office or other groups.
- To formulate advance directives.
- To request a state hearing, including information on the circumstances under which an expedited hearing is possible.
- To access Minor Consent Services.
- To receive written member-informing materials in alternative formats (such as braille, large-size print, and audio format) upon request and in a timely fashion appropriate for the format being requested and in accordance with Welfare & Institutions Code Section 14182 (b)(12).
- To be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience, or retaliation.
- To receive information on available treatment options and alternatives, regardless of cost or benefit coverage, presented in a manner appropriate to your condition and ability to understand.
- To have access to and receive a copy of your medical records, and request that they be amended or corrected, as specified in 45 Code of Federal Regulations §164.524 and 164.526.
- Freedom to exercise these rights without adversely affecting how you are treated by HPSM, your providers or the State.
- To have access to family planning services, Freestanding Birth Centers, Federally Qualified Health Centers, Indian Health Service Facilities, midwifery services, Rural Health Centers, sexually transmitted disease services and Emergency Services outside HPSM’s network pursuant to the federal law.
- To make recommendations about HPSM’s member rights and responsibilities.
HPSM members have these responsibilities:
- Carefully read all HPSM Member materials so that you understand how to use your benefits and what procedures to follow when you need care.
- Do your best to keep provider appointments; if you need to cancel or reschedule an appointment, call your provider at least 24 hours in advance or as soon as possible.
- Show your HPSM ID card or remember to tell your provider (your doctor, hospital, or pharmacy) that you are an HPSM member before receiving care.
- Follow the treatment plan that you and your provider have agreed upon.
- Provide accurate and complete information about your health care needs to HPSM and to your provider. Tell your provider if you have a medical condition.
- As best as you can, understand your health care needs and participate in developing treatment plans and goals with your providers.
- Follow the plans and instructions for care that you have agreed upon with your provider. Ask your provider questions if you do not understand something or are not sure about the advice that you are given.
- See specialists to whom your primary care provider refers you.
- Actively participate in health care programs that keep you well.
- Work with your providers to build and maintain a good working relationship.
- Use the emergency room only in case of an emergency or as directed by your provider.
- Follow-up with your primary care provider after getting care at an emergency facility.
- Report lost or stolen ID cards to HPSM Customer Support and do not let anyone else use your HPSM ID card.
- Call HPSM Customer Support if you do not understand how to use your benefits or have any problems with the services that you received.
- Tell HPSM if you move and/or change your phone number. Call HPSM Customer Support and the San Mateo County Human Services Agency. If you receive SSI, call Social Security Administration. We all need to have your correct address and phone number on file.
- Follow the HPSM grievance procedure if you want to file a complaint.
- Treat all HPSM staff and your health care providers respectfully and courteously.
Missed Appointments
HPSM advises members if they cannot keep an appointment, they need to call their provider to cancel or reschedule the appointment as soon as possible. Providers can send HPSM Provider Services information about members that have missed multiple appointments. HPSM staff will contact the member and remind the member about the importance of calling to cancel appointments in advance.
Provider Selection
Primary Care Physician (PCP)
An HPSM member’s care is managed by the member’s assigned PCP. A PCP may be a pediatrician, a general practitioner, a family practitioner, an internist, a Federally Qualified Health Care Clinic (FQHC), a Native American health service provider, a nurse practitioner, or in some cases, an OB/GYN provider.
Women’s Services – OB/GYN Services
Female HPSM members have unlimited, direct access to OB/GYN services. Members may choose to have these services provided by the PCP or members may self-refer to any contracted OB/GYN or PCP within the HPSM network for OB/GYN services.
Pregnancy Care
HPSM encourages pregnant women to get early prenatal care. Members may select an Obstetrician or Certified Nurse Midwife for care during pregnancy. Members have the right to select Certified Nurse Midwife services from an out-of-plan Medi-Cal Provider if they are not available through HPSM.
Indian Health Services
American Indians or Alaskan Natives who are HPSM members may choose any available Indian Health Service Provider available, as provided under Federal Law. The provider does not have to be an HPSM network provider and HPSM will arrange to coordinate appropriate services for these members.
Doula Benefit
HPSM provides doula benefits for prenatal members, and postpartum members up to 12 months after delivery. Doula services can be provided to HPSM Medi-Cal, CareAdvantage and HealthWorx (HMO) members virtually or in-person in any settings including, but not limited to, homes, office visits, hospitals during labor, or alternative birth centers. Additional information regarding member eligibility for doula services can be found in, “Section 6: Ancillary Services” of the Provider Manual.
Primary Care Physician (PCP) Selection Process
HPSM members are encouraged to self-select a PCP as soon as they become eligible for or are enrolled in an HPSM program. Member Services Representatives and CareAdvantage Navigators are available to assist members with the PCP selection process. HPSM members can also select a PCP in the HPSM Member Portal.
When Medi-Cal members become HPSM eligible, “New Member Guides” are mailed to the member, requesting that they select a PCP. New HPSM Medi-Cal members are not assigned to a PCP for the first 30 days of their HPSM eligibility to allow them time to self-select a PCP. Members who do not self-select a PCP are automatically assigned to a PCP (see below for more information) according to the guidelines prescribed by the California Department of Health Care Services. Members that have primary other health coverage, including Original Medicare are not assigned to a PCP.
New HPSM members in other programs (CareAdvantage, HealthWorx and ACE) are required to select a PCP as part of their initial enrollment process.
Auto-Assignment to a PCP (for Medi-Cal members only)
If a Medi-Cal member does not self-select a PCP within the first 30 days of HPSM enrollment, the member will be auto-assigned to a PCP based on geographic location, member age and PCP capacity.
If a member is auto assigned to a PCP, the member is informed that they have the option to change their assigned PCP.
Changing Primary Care Providers
Members can request a PCP change at any time by calling HPSM Customer Support. Members can also change their PCP in the HPSM Member Portal.
HPSM must receive requests for PCP changes by the last day of the current month. PCP changes are effective the 1st of the following month. Medi-Cal, HealthWorx and ACE members will receive a confirmation letter with the name of the new PCP. Only CareAdvantage members will receive a new HPSM ID card with the name of their new PCP.
Provider Request for Member Reassignment
Physician requests for member reassignment to the care of another provider must be pre-approved by the HPSM Chief Medical Officer or designee. Physicians requesting member reassignment must complete a Provider Request for Member Reassignment form. The form must include documentation of the reasons for the request and actions taken to resolve the issues with the member. The form and any attachments can be emailed to HPSM Provider Services at [email protected] or sent via fax to 650-616-8046.
The provider should not notify the member that a request for reassignment has been submitted to HPSM. The Provider Request for Member Reassignment form will be reviewed by HPSM’s Chief Medical Officer (CMO)or designee. Provider Services will notify the provider in writing within 14 business days of the CMO or designee’s decision to approve or deny the request.
HPSM follows regulatory guidelines and retains sole and final authority to review and act upon the requests from providers to terminate a member. Members are not transferred against their will until HPSM carefully reviews the matter, determines that transfer is appropriate, and confirms that HPSM’s internal procedures have been followed.
All reassignment requests are carefully reviewed, and care is taken to preserve member rights against discrimination due to age, race, gender, or health status.
If the reassignment is approved, HPSM will send a letter to the member (certified, return receipt). The reassignment notification letter will inform the member that a reassignment request was made by the primary care physician and that the member can select another. The letter outlines the reasons why the request was made and informs the member that if they do not select a new primary care physician within 30 days of the date the letter was mailed, the member will be auto assigned to a new one.
The member will be reassigned from the requesting provider once the written notice is sent to the member and is effective the first of the following month. When a member is assigned to a new primary care physician, the previous provider must supply patient records, reports, and other documentation at no charge to the new one. The transferring provider must continue to coordinate care through the end date of the reassignment.
Providers Leaving the Network
HPSM will provide continuity of care for covered services rendered to a member by a provider whose HPSM affiliation has ended in the following circumstances:
- An acute condition: completion of covered services will be provided for the duration of the acute condition.
- A serious chronic condition: Completion of covered services for a period necessary to complete a course of treatment and to arrange for a safe transfer to another HPSM provider, as determined by HPSM in consultation with you and the terminated provider and consistent with good professional practice. Completion of covered services shall not exceed 12 months from the date that the provider left HPSM.
- A pregnancy: Including postpartum care, for the duration of the pregnancy.
- A terminal illness: Completion of covered services for the duration of the terminal illness.
- A surgery or other procedure: approved by HPSM as part of a documented course of treatment and occurs within 180 days from the date that the provider left HPSM.
- Covered services for a child: the child should be between ages birth and 36 months for up to 12 months from the date that the provider left HPSM.
The terminating provider must agree in writing to provide services to a member in accordance with the terms and conditions, including reimbursement rates, of his or her agreement with HPSM prior to termination.
HPSM does not provide continuity of care services if:
- The provider is unwilling to continue to treat the member or accept HPSM’s payment or other terms.
- HPSM discontinued a contract based on a professional review action or a medical disciplinary cause or reason or for fraud or other criminal activity.
- Services are not covered by HPSM.
- The continuity of care request is for Durable Medical Equipment, transportation or other ancillary services or carved-out service.
Programs and Enrollment Information
Medi-Cal is California’s Medicaid health care program. Medi-Cal covers a variety of medical services for children and adults with limited income and resources. Eligibility is determined by the San Mateo County Human Services Agency or through Supplemental Security Income (SSI) administered by Social Security Administration (SSA). Eligibility information is available at the Human Services Agency website. Prospective members can also call the San Mateo County Human Services Agency at 1-800-223-8383 to find out if they are eligible to receive Medi-Cal health benefits.
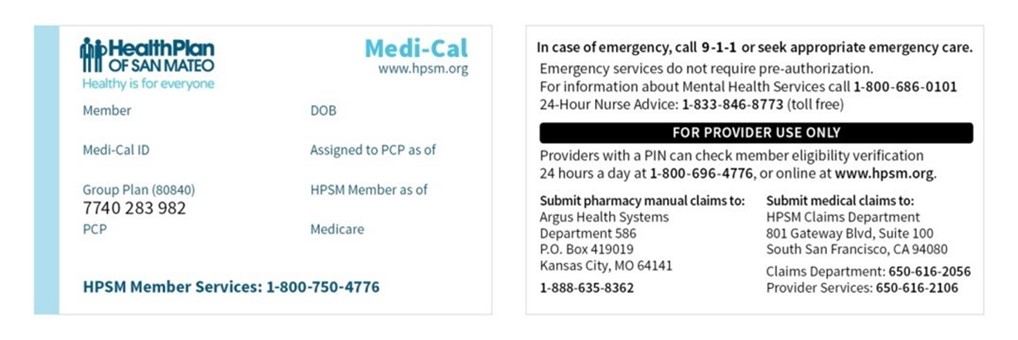
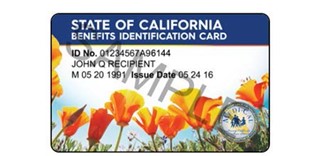
Medi-Cal eligible beneficiaries with qualifying Medi-Cal aid codes are automatically enrolled in HPSM. Every HPSM Medi-Cal member receives an HPSM ID card and a Medi-Cal Benefits Identification Card
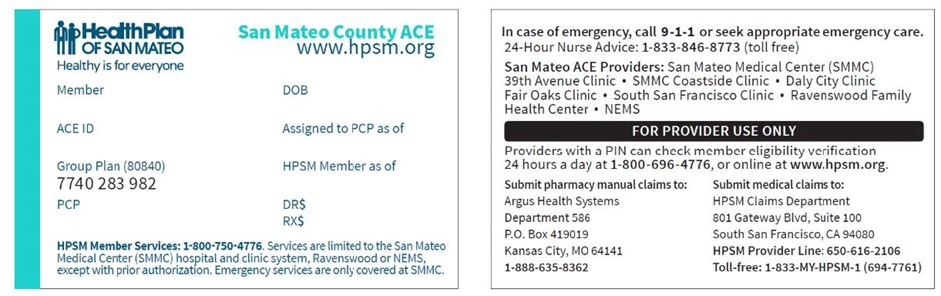
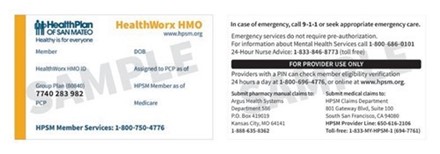
(BIC) issued by DHCS. Sample ID cards are included later in this section.
Types of Medi-Cal Members
PCP-Assigned Members
These are members that are assigned to a Primary Care Provider (PCP) and appear on the PCP’s case management list
Unassigned Members
Unassigned members are not assigned a PCP and do not require referrals to see contracted, in-network PCPs. Members that have Other Health Coverage (OHC), including Original Medicare, in addition to Medi-Cal are not assigned to a PCP; the OHC is usually the member’s primary coverage.
Share of Cost Members
Some Medi-Cal recipients must pay, or agree to pay, a monthly dollar amount toward their medical expenses before they qualify for Medi-Cal benefits. This amount is called the Medi-Cal Share-of-Cost (SOC). A Medi-Cal recipient’s SOC is like a private insurance plan’s out-of-pocket deductible. Share-of-Cost members are not assigned to a PCP.
Medi-Cal recipients with a SOC are not eligible for full-scope Medi-Cal until they have met their SOC amount for the month. Members with a Medi-Cal SOC appear in suspense status in the HPSM Provider Portal.
After a recipient meets the SOC for the month, HPSM will pay for covered medical expenses for the rest of the month. More information about the Medi-Cal SOC, including how a provider should collect and clear a share of cost, can be found on the Medi-Cal Provider website.
Whole Child Members
The Whole Child Model is a partnership between HPSM and San Mateo County to deliver coordinated care and services to eligible children with complex medical conditions. The Whole Child Model was known as the California Children’s Services (CCS) Pilot until 2018.
HPSM Medi-Cal members under 21 years old who are eligible for CCS are enrolled into the Whole Child Model program. These HPSM Medi-Cal members receive a dedicated case manager who oversees the member's total care. This includes coordinating medical, social, and mental health services for the member or their family as needed.
For more information about the Whole Child Model and to make a referral, call the San Mateo County CCS staff at 650-616-2500.
CareAdvantage Dual Eligible Special Needs Plan (D-SNP)
CareAdvantage is a Medicare Advantage-Prescription Drug (MA-PD) plan for people who have both Medicare and Medi-Cal. CareAdvantage contracts with both Medicare and Medi-Cal to provide benefits of both programs to enrollees with the goal of a seamless service delivery experience for D-SNP beneficiaries. To enroll in CareAdvantage, members must have Medicare Part A (hospital insurance) and Part B (medical insurance), full-scope Medi-Cal through HPSM and must live in San Mateo County.
Members that want to enroll in CareAdvantage should call a licensed HPSM CareAdvantage Medicare Specialist at 1-888-252-3153 or 650-616-1500.
Enrollment in CareAdvantage is optional. Some members with Medicare and Medi-Cal may decide to remain in Original (fee for service) Medicare and enroll in a Part D Prescription Drug Plan (PDP) or join another Medicare Advantage Plan. The member will keep his/her HPSM Medi-Cal eligibility but will not be enrolled in CareAdvantage.
Anyone with questions about Medicare can call the San Mateo County Health Insurance Counseling and Advocacy Program (HICAP) at 1-800-434-0222.
HealthWorx
HealthWorx is an employer group health insurance program. HealthWorx enrollment is limited to San Mateo County Public Authority In-Home Support Services (IHSS) workers and City of San Mateo Per Diem employees. HealthWorx only covers the employee; it does not cover family members.
For more information, IHSS Workers should call the San Mateo County Public Authority at 650-573-3733. City of San Mateo part-time employees should call SEIU at 650-801-3501 (English); 650-801-3502 (Spanish) or 650-801-3503 (Chinese).
San Mateo County ACE Program
The San Mateo County ACE (Access and Care for Everyone) Program is a county-sponsored program that provides health care coverage to uninsured residents of San Mateo, age 19 and older, with low income. HPSM administers the San Mateo ACE Program under a contract with San Mateo County. Prospective enrollees can call the Health Coverage Unit at 650-616-2002 for more information.
San Mateo County ACE is not insurance. The San Mateo County ACE Program covers a wide range of health care and pharmacy benefits under a coordinated system of care, but it is not an insurance product subject to state insurance requirements. It is a payer of last resort, which means it pays only for certain services that are not covered by other existing coverage programs. Services are primarily provided through the San Mateo Medical Center (SMMC), North East Medical Services (NEMS) and the Ravenswood Family Health Center.
ACE enrollees can only receive emergency services at SMMC.
Identifying HPSM Members
HPSM members are enrolled in either Medi-Cal, CareAdvantage Dual Eligible Special Needs Plan (D-SNP), HealthWorx, or San Mateo County ACE. All HPSM members have an HPSM ID card showing the program that they are enrolled in. Examples of HPSM ID cards can be found later in this section.
PCP Active Engagement Reports
Lists of empaneled patients are published once monthly for each primary care clinic. These “Active Engagement Reports” are available for download in HPSM’s eReports portal and include all members assigned to the PCP that month and information such as assigned member name, HPSM ID number, preferred language, program, date assigned to the PCP, contact information, and some utilization information. For more information on registering for or using eReports, please reference the eReports User Guide – Primary Care.
Member Eligibility
Providers should verify HPSM member eligibility at the time of each visit. A member's eligibility can change at any time for any number of reasons, including a change in Medi-Cal status or change in residence address.
How to Check Eligibility
Monthly Active Engagement Reports for Primary Care Physician (PCPs)
PCPs should check for the member's name on the list published to eReports and available for download at the beginning of the month. For more information on how to register for or use eReports, refer to the eReports User Guide – Primary Care."
eReports Portal
Providers can verify member’s eligibility, submit claims using eHEALTHSuite and check payment status on the provider portal. To register, visit the Provider Portal.
Medi-Cal’s 24-Hour State Automated Eligibility Verification System
Medi-Cal members only: 1-800-456-2387.
Medi-Cal DHCS Website
Medi-Cal and Medicare/Medi-Cal members only. Eligibility information is available on California’s Medi-Cal website. For assistance in obtaining a login and password for the State of California Medi-Cal website, please call the POS/Internet Help Desk at 1-800-427-1295 for more information.
Medi-Cal Point of Service (POS) Device
Swiping the patient’s Medi-Cal Beneficiary Identification Card (BIC) in the State’s POS device will also enable you to determine eligibility. The POS device provides eligibility as well as Share-of-Cost liability information for dates of service within the prior 12 months. To learn more, please call the DHCS Telephone Service Center at 1-800-541-5555.
Please remember that verification of active enrollment is subject to retroactive adjustment in accordance with the terms and conditions of coverage described in the member's benefit plan.
Specialist providers, hospitals, and other service providers should also verify eligibility on the date that the service is rendered. A referral or authorization does not guarantee that the member is eligible on the date of service.
ID Cards by Line of Business
Medi-Cal ID Card
CareAdvantage ID Card

Medi-Cal Benefits ID Card (BIC)
HealthWorx ID Card
ACE Program ID Card